Bro Science Saves Lives: Hypogonadism
An Introduction to Testosterone Deficiency and Its Implications
To ignore the full spectrum of benefits arising from optimized male hormone levels is dangerously myopic. As a hormone whose deficiency can provoke depression/anxiety, impair fertility, worsen obesity, exacerbate insomnia, reduce bone and muscle density, Testosterone should be at the center of our understanding of chronic disease. Research shows a downward trending slope of lower and lower average T-levels in recent decades. We can also look to the rising rates of ED in young men, and the strategic rebranding of erection aids and hair loss treatments for younger audiences as signs that we are simply not the same men our fathers and grandfathers were. An acute awareness of this essential hormone shouldn’t be reserved for gym-bros. Dialing in T-levels should be a priority for every man interested in experiencing the fullness of his own physiology and maximization of his potential
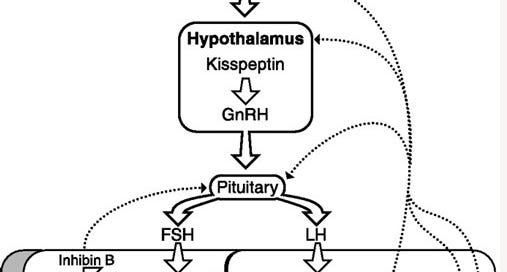
Before exploring the vast implications of hypogonadism (low-T) lets first explore how our body produces T. The magic show takes place within the Hypothalamic-Pituitary-Testicular Axis (HPTA abbrv). Our HPTA is the pathway through which our balls and brain communicate. Our hypothalamus uses Gonadotropin-Releasing Hormone (GnRH) to tell our pituitary gland to release Luteinizing Hormone (LH) and Follicle Stimulating Hormone (FSH) stimulating testicular activity. Like a game of telephone, the biochemical call to action reaches our gonads where LH stimulates gonadal Leydig cells to release T and FSH stimulates spermatogenesis. T can convert into Dihydrotestosterone via the enzyme 5-alpha-reductase or into Estradiol/Estrogen via the enzyme aromatase. The hypothalamus maintains an acute awareness of circulating T levels to gauge the subsequent rate and rhythm of production (this is what endocrinologists refer to as Negative Feedback). Being cyclical in nature, any impedance to the circuit has a systemic impact.
Hypogonadism can have a variety of congenital causes, and to a certain degree is normal with age, but a great deal of premature HPTA interference stems from lifestyle factors. Similarly, the line between cause and effect with regards to low T is blurry, resulting in viscous cycles that lead us deeper into hormonal misalignment.
Allopathic medicine takes a mechanistic approach to understanding and treating the body. Our physiology is taxonomized into distinct systems; each having their own medical specialities. A great deal of focused care is made possible as each specialist is able to master their anatomical milieu. On the flipside however the interconnectedness of our physiology is obfuscated. Viewing the body as a “machine” may be a beneficial metaphor, but the map is not the territory. We are miracles of nature with the gift of sentience to be able to recognize our own mystery. Understanding this is critical in that it allows us to get beyond viewing disease processes as simple “cause and effects.” In an earlier article we talked about Metabolic Syndrome (the co-concurrence of insulin resistance, obesity, hypertension, and impaired lipid function) and how each specific component exists inseparable from one another. New research is shining light on the relation between Low-T and MetS. Improvement in insulin resistance and body composition are noted with exogenous Testosterone Replacement Therapy (TRT) in hypogonadal men. Additionally the controlled inhibition of T in cancer patients was shown to increase the risk for diabetogenic disease.
“Findings from men undergoing androgen suppression as treatment for prostate cancer confirm that the hypogonadal state increases body fat mass and serum insulin and there is a high rate of developing new diabetes in this population”(Frontiers of Hormone Research).
The link between metabolic dysfunction and hypogonadism is so strong we can find it epigenetically across generations. Impaired metabolic health of a father can contribute to inherited hypogonadism in the son. This shouldn’t scare us into inaction. The beauty of epigenetics is that it shows us how much good can be done through lifestyle intervention.
Beyond metabolic health, T levels play a significant role in regulating mood, and can be a determinant for mental health. The interconnectedness of distinct body “systems” is so deep the new field of psychoneuroendocrinology has been established to explore overlapping pathways. The dance of Testosterone and Cortisol is interesting, and our current understanding is pretty non-linear. Machine metaphors of the body continue to fail in adequately explaining its intricacy. Input→Output can only get us so far. Some research indicates that Testosterone attenuates Cortisol, making us more resilient to the effects of chronic stress, however this buffering effect is theorized to be context dependent. Men with higher levels of testosterone may notice increased stress hormone signaling when the stressor relates to perceived social status. Endogenous Testosterone (produced naturally within the body) is noted to play a protective role in mood regulation. No doubt this explains why low T often leads to depressive symptomatology, and why supraphysiological T-levels (in instances of anabolic steroid use for example) can lead to drastic changes in one's psychosocial landscape. Additionally depressive moods noted following traumatic brain injury are the result of structural damage to the HPTA. Dr. Andrew Huberman of Stanford University Neurobiology, is quoted saying “Testosterone makes effort feel good.” No surprise here T deficiency is correlated with loss of interest in life.
The point being; it’s all connected. Our gut, brain, and balls work as one. A seemingly simple truth that often goes ignored by current standards and guidelines of medical intervention. Although the lack of simple cause/effect explanations for sickness may seem daunting, it points us towards multiple possibilities for healing. Medical specialization has its utility, but if we continue to mistake the map for the territory we are bound to get lost. Additionally we have fallen prey to a medical system that relates to health as “the absence of acute sickness”, when in reality it could mean so much more.
I don’t want you to be “not-sick”. I want you to feel fucking fantastic in your own body. This is your birthright.
Lifestyle intervention is an incredibly potent means through which we can unfuck ourselves. Yet the medical establishment fails to adequately address it. The intention for future articles is to fill in that gap. We’ll explore sleep, nutrition, exercise, and mindset as ways we can step fully into our own body, empowering us to conquer each day. Stay tuned.
References:
Priskorn L, Jensen TK, Bang AK, Nordkap L, Joensen UN, Lassen TH, Olesen IA, Swan SH, Skakkebaek NE, Jørgensen N. Is Sedentary Lifestyle Associated With Testicular Function? A Cross-Sectional Study of 1,210 Men. Am J Epidemiol. 2016 Aug 15;184(4):284-94. doi: 10.1093/aje/kwv338. Epub 2016 Aug 8. PMID: 27501721.
Zoeller RT, Tan SW, Tyl RW. General background on the hypothalamic-pituitary-thyroid (HPT) axis. Crit Rev Toxicol. 2007 Jan-Feb;37(1-2):11-53. doi: 10.1080/10408440601123446. PMID: 17364704.
https://www.healthline.com/health/side-effects-of-low-testosterone#sexual-function
Sizar O, Schwartz J. Hypogonadism. [Updated 2021 Jun 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532933/
https://my.clevelandclinic.org/health/diseases/15603-low-testosterone-male-hypogonadism
Carrageta DF, Oliveira PF, Alves MG, Monteiro MP. Obesity and male hypogonadism: Tales of a vicious cycle. Obes Rev. 2019 Aug;20(8):1148-1158. doi: 10.1111/obr.12863. Epub 2019 Apr 29. PMID: 31035310.
Corona G, Rastrelli G, Dicuio M, Concetti S, Minnetti M, Pivonello R, Isidori A, Sforza A, Maggi M. Subclinical male hypogonadism. Minerva Endocrinol (Torino). 2021 Sep;46(3):252-261. doi: 10.23736/S2724-6507.20.03208-3. Epub 2020 Sep 24. PMID: 32969626.
Crisóstomo L, Pereira SC, Monteiro MP, Raposo JF, Oliveira PF, Alves MG. Lifestyle, metabolic disorders and male hypogonadism - A one-way ticket? Mol Cell Endocrinol. 2020 Oct 1;516:110945. doi: 10.1016/j.mce.2020.110945. Epub 2020 Jul 22. PMID: 32707080.
Mihalca R, Fica S. The impact of obesity on the male reproductive axis. J Med Life. 2014 Jun 15;7(2):296-300. Epub 2014 Jun 25. PMID: 25408743; PMCID: PMC4197498.
https://www.urologytimes.com/view/testosterone-levels-show-steady-decrease-among-young-us-men
Nieschlag E, Nieschlag S. Testosterone deficiency: a historical perspective. Asian J Androl. 2014;16(2):161-168. doi:10.4103/1008-682X.122358
Knight, Erik L et al. “Exogenous testosterone enhances cortisol and affective responses to social-evaluative stress in dominant men.” Psychoneuroendocrinology vol. 85 (2017): 151-157. doi:10.1016/j.psyneuen.2017.08.014
Plourde V, Daya H, Low TA, Barlow KM, Brooks BL. Evaluating anxiety and depression symptoms in children and adolescents with prior mild traumatic brain injury: Agreement between methods and respondents. Child Neuropsychol. 2019 Jan;25(1):44-59. doi: 10.1080/09297049.2018.1432585. Epub 2018 Jan 30. PMID: 29382257.
McHenry J, Carrier N, Hull E, Kabbaj M. Sex differences in anxiety and depression: role of testosterone. Front Neuroendocrinol. 2014 Jan;35(1):42-57. doi: 10.1016/j.yfrne.2013.09.001. Epub 2013 Sep 24. PMID: 24076484; PMCID: PMC3946856.
Brand JS, van der Tweel I, Grobbee DE, Emmelot-Vonk MH, van der Schouw YT. Testosterone, sex hormone-binding globulin and the metabolic syndrome: a systematic review and meta-analysis of observational studies. Int J Epidemiol. 2011 Feb;40(1):189-207. doi: 10.1093/ije/dyq158. Epub 2010 Sep 24. PMID: 20870782.
The Science of How to Optimize Testosterone & Estrogen | Huberman Lab Podcast #15